Lumbar Spine
Low Back Pain and Surgical Intervention
Acute low back pain is common. The type of pain can range from an ache to shooting pains or spasms. It can last up to three months, but most people feel better in a few days or weeks. Acute low back pain is often described as ‘non-specific’, meaning the cause is unknown or uncertain. It is thought to be associated with the muscles, ligaments or joints in the back. Acute low back pain is rarely due to any serious injury, disease or damage to the spine and does not cause lasting damage. It’s possible to have acute low back pain once, which gets better and never returns. But it’s more likely you will experience another episode in the future.
Most people with low back pain do not require X-rays, CT scans or MRI scans, and most people with low back pain do not need any surgery. Read more >>
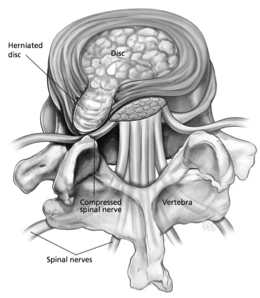
Lumbar discectomy is a surgical procedure to remove part of a disc that is pressing on spinal nerves in the lower (lumbar) back.
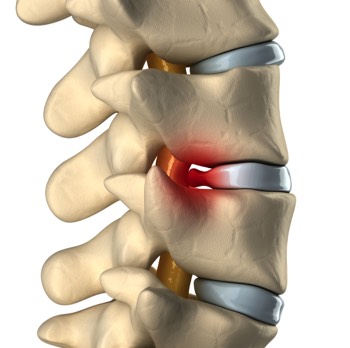
Discs are soft but strong, thick cushions that sit between each vertebra of the spinal column. They are resilient to the mechanical forces placed on them but can become damaged through age or trauma, such as heavy lifting. This damage is called “herniation”. (A disc hernia is often called a disc prolapse or a slipped disc.)
When a disc herniates, the protrusion may press into the spinal canal or on a nearby spinal nerve, compressing or “pinching” it.
The most common symptoms are pain in the lower back, buttocks, hip, thigh and leg, numbness, tingling and weak- ness in the legs. In serious cases, bladder and bowel control may be impaired or lost.
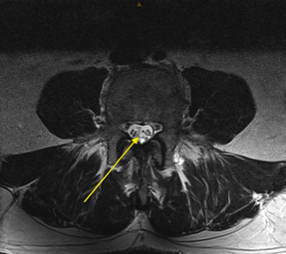
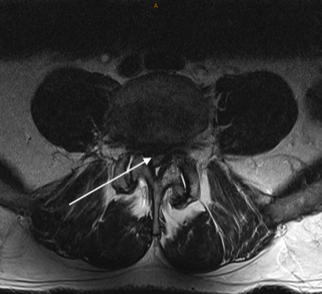
A large herniation of a lumbar disc, most commonly between the fourth and fifth lumbar vertebrae, can exert severe pressure on spinal nerves within the spinal canal. In rare cases, this may become a medical emergency, and surgery is needed to stop the pressure caused by the herniated disc.
Diagnosis
Diagnostic imaging of discs and the spinal column can provide Prof Davis with important information about any abnormalities. Magnetic resonance imaging (MRI) can reveal the anatomy of a herniated disc and the precise location of nerve compression.
Professor Davis will examine you to determine your strength, reflexes, ability to feel pain, and ability to move. You will be asked about pain, numbness, weakness, previous similar symptoms, and any bowel or urinary problems.
Your medical history
Prof Gavin Davis needs to know your medical history to plan the best treatment for you. Tell him about any health problems you have. Some may interfere with treatment, surgery, anaesthesia or recovery.
These include “wait and see”, pain-relieving medications, foraminal block (local anaesthetic injection), physical therapy and surgery (discectomy). Most discectomies are now performed as microdiscectomies.
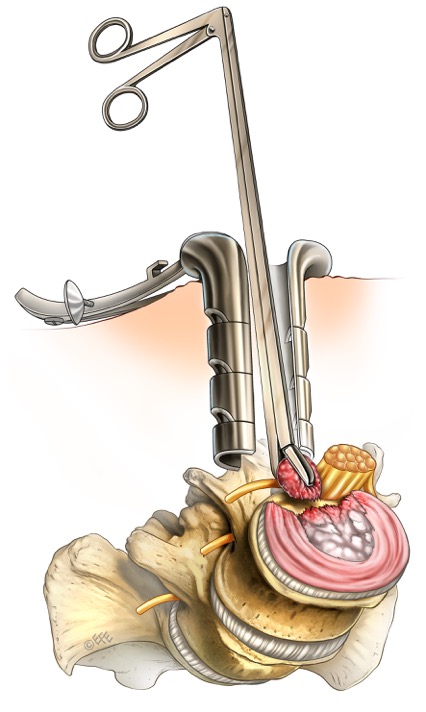
A microdiscectomy involves a very small incision in the lower back, and using X-ray guidance and microsurgery to expose the underlying disc prolapse and adjacent nerves, and removing the fragment of herniated disc, whilst protecting and preserving the nerves. The aim of surgery is to take all the pressure off the nerve(s), thus relieving the patient of leg pain (sciatica). This usually provides sufficient relief to enable the patient to then continue with gentle physiotherapy and exercises focused on back stability and strengthening, including core stability.
A decision to have discectomy: As you make the decision whether to have surgery, make sure that you understand the risks, benefits and limitations of discectomy.
There can be risks if you do not have surgery to relieve compression of a spinal nerve because further damage may occur. In some patients, the most serious complications can include further pain, numbness, paralysis or loss of bladder or bowel control.
Lumbar Microdiscectomy
Spinal canal stenosis involves narrowing of the space available for the nerves (the spinal canal), which may cause nerve pain, or limitation of walking distance (known as spinal claudication). When this occurs, it is often progressive, such that that the patient’s walking distance becomes shorter and shorter over time, and in extreme cases, limits walking altogether. Whilst physiotherapy is the appropriate treatment in early and mild forms of this condition, when the symptoms are more advanced, then surgery is required.
Surgery involves removal of any bone, spurs and ligament that are compressing the nerves. This is known as Decompressive Laminectomy. In most cases, this results in restoration of walking function, after a sufficient period of rehabilitation.
In some cases, there is a risk that the decompressive laminectomy will worsen some intrinsic spinal instability. Therefore, to prevent further worsening of this instability, a fusion is required. Fusion is generally considered in two forms: instrumented and non-instrumented.
Non-instrumented fusion means using some of your bone, or a synthetic bone substitute, placed along the side of the spine, to add an extra layer of support, and reduce movement at that level, providing increased spinal stability. Instrumented spinal fusion is similar to this, but in addition to the bony fusion, metal screws and rods are used to provide an additional level of support.
The type of surgery that you require depends on the findings on your MRI and X-rays, and will be discussed with you during your appointment with Professor Davis.
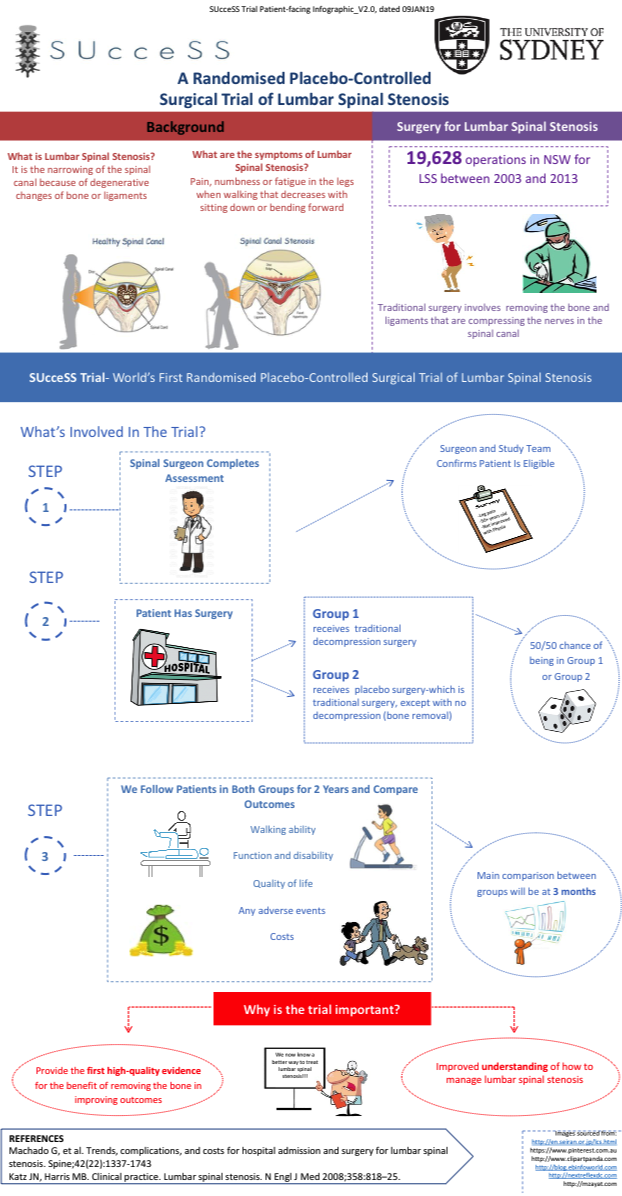
SUcceSS
SUcceSS is the world’s first randomised placebo-controlled study of decompression surgery for central lumbar canal stenosis conducted at the University of Sydney. The study is being conducted in Sydney and Melbourne. For more information click here

Only you can decide if surgery is right for you. If you have any questions, please ask Professor Davis.
Anaesthesia: Lumbar spinal surgery is performed under general anaesthesia.
Possible risks and complications: Whilst modern spinal surgical procedures are generally safe, they do have risks of side effects. Although uncommon, complications are possible.
These are more fully outlined in the complete NSA patient education pamphlet and should be discussed with Prof Gavin Davis.
Spinal Tumours include those in the bone (vertebral body), those around the spinal cord and nerves (extradural) and those in the spinal cord and nerves (intradural). Different tumours require different treatment.
For example -
- Benign tumours that are not growing or causing symptoms: these may be observed with serial MRI scans
- Benign tumours that are growing or causing symptoms: these require surgery to remove
- Malignant tumours: these may require surgery, chemotherapy and/or radiotherapy
Some of the spinal tumours that are more commonly operated on include meningiomas, schwannomas, neurofibromas and ependymomas, although there are many other types of tumours that also require surgery. Each case is carefully assessed by Prof Davis, and the most appropriate treatment plan is developed with you.
If you have any questions about your spinal tumour, please contact Prof Davis.